Metformin has been the go-to pill for type 2 diabetes for over 60 years. It’s cheap, safe, and works well for most people. But if you’ve been on it for a while and still aren’t hitting your blood sugar goals-or if you’re dealing with stomach issues, weight gain, or heart problems-you’re not alone. More and more doctors are turning to newer options. It’s not that metformin is outdated. It’s just that we now have better tools for people who need more than what metformin can offer.
Why are people looking for alternatives to metformin?
Metformin doesn’t work for everyone. About 20% of people can’t take it because of nausea, diarrhea, or vitamin B12 deficiency. Others find it doesn’t lower their A1c enough, even at the highest dose. And for those with heart failure, kidney disease, or who need to lose weight, metformin just doesn’t cut it anymore.
Recent studies show that even when metformin is working, many patients still end up needing insulin within 5 to 7 years. That’s not failure-it’s just how the disease progresses. The goal now isn’t just to lower blood sugar. It’s to protect the heart, kidneys, and help with weight loss. Newer medications do all three.
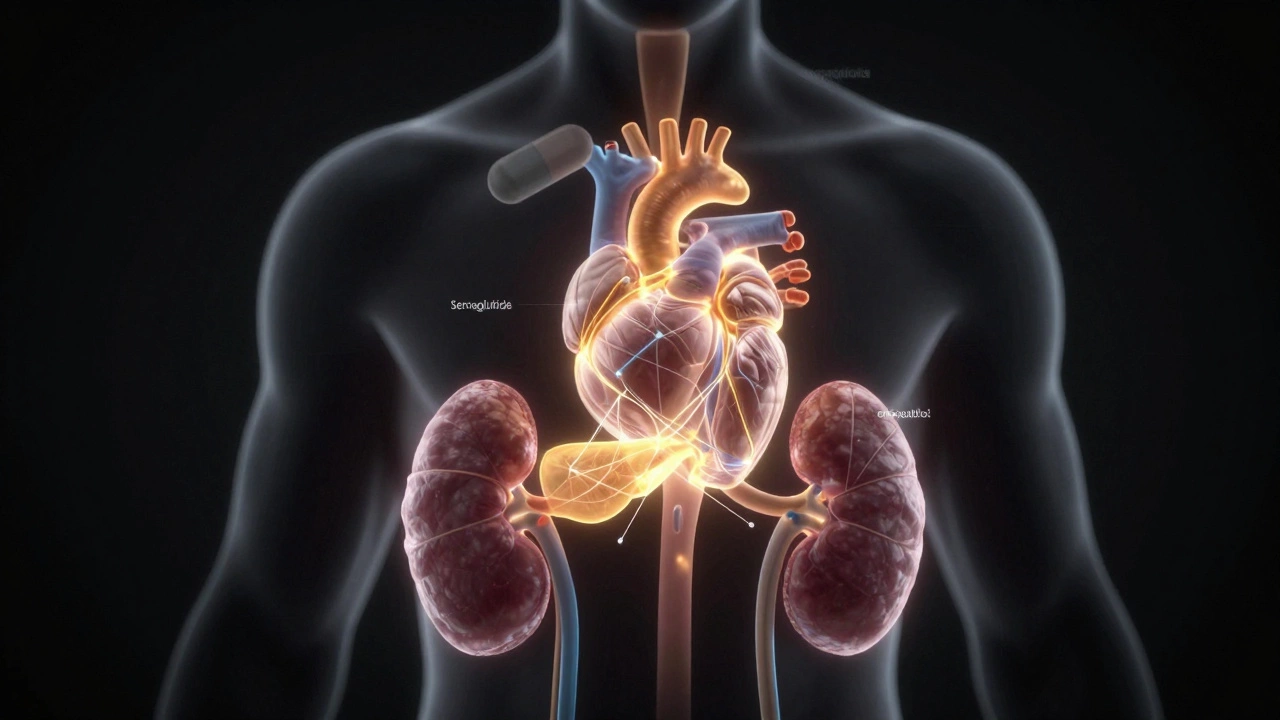
GLP-1 receptor agonists: The biggest shift in diabetes care
The most talked-about replacements for metformin are GLP-1 receptor agonists. These include drugs like semaglutide (Ozempic, Wegovy), liraglutide (Victoza), dulaglutide (Trulicity), and tirzepatide (Mounjaro, Zepbound).
These aren’t just blood sugar pills. They’re injectables that mimic a natural hormone in your gut that tells your pancreas to release insulin only when needed. They also slow digestion, reduce appetite, and help you lose weight-often 10 to 20 pounds or more.
In the STEP trials, people using semaglutide lost an average of 15% of their body weight. That’s more than most bariatric surgeries. And in the LEADER and REWIND trials, these drugs cut heart attacks, strokes, and death from heart disease by 20-26%.
Doctors are now starting patients on GLP-1 agonists right after diagnosis if they have heart disease, obesity, or kidney problems-even before metformin. That’s a huge shift.
SGLT2 inhibitors: Protecting kidneys and the heart
Another group of drugs that’s replacing metformin in many cases are SGLT2 inhibitors. These include empagliflozin (Jardiance), dapagliflozin (Farxiga), and canagliflozin (Invokana).
They work by making your kidneys flush out extra sugar through urine. That lowers blood sugar naturally. But the real win? They reduce the risk of heart failure hospitalization by 30% and slow kidney disease progression by up to 40%.
In the EMPA-REG OUTCOME trial, people with diabetes and heart disease who took empagliflozin had a 38% lower risk of dying from heart problems. Similar results came from the DAPA-HF and CREDENCE trials.
These are now first-line for people with heart failure or chronic kidney disease-even if their A1c is only slightly high. You don’t need to fail metformin first. If your heart or kidneys are at risk, these drugs are the new starting point.

How do these compare to metformin?
Here’s how the newer drugs stack up against metformin:
| Medication | How it lowers blood sugar | Weight effect | Heart protection | Kidney protection | Side effects |
|---|---|---|---|---|---|
| Metformin | Reduces liver glucose output | Neutral or slight loss | Mild benefit | No proven benefit | Stomach upset, B12 deficiency |
| GLP-1 agonists | Stimulates insulin, slows digestion | Significant loss (10-20 lbs+) | Strong benefit (20-26% risk reduction) | Moderate benefit | Nausea, vomiting, rare pancreatitis |
| SGLT2 inhibitors | Removes sugar through urine | Mild loss (5-10 lbs) | Strong benefit (30% heart failure reduction) | Strong benefit (up to 40% slower decline) | Yeast infections, dehydration, rare foot amputations |
Metformin still wins on cost-it’s under $10 a month. But GLP-1 agonists and SGLT2 inhibitors are now available as generics in many countries. Even at full price, their long-term savings from preventing heart attacks, dialysis, or amputations often outweigh the cost.
Who should switch from metformin?
You might be a good candidate for switching if:
- Your A1c is still above 7.5% on max metformin dose
- You have heart disease, heart failure, or kidney disease
- You’re overweight or obese and struggling to lose weight
- You can’t tolerate metformin’s stomach side effects
- You’re on insulin and want to reduce doses
But not everyone needs to switch. If metformin keeps your blood sugar in range, you’re not overweight, and you feel fine-there’s no rush. It’s still a great drug for many.
What about newer oral options?
There’s also a new class called dual GIP/GLP-1 agonists-tirzepatide (Mounjaro, Zepbound) is the first. It’s a single injection that hits two hormones at once. In trials, it lowered A1c by up to 2.4% and helped people lose over 20% of their body weight. It’s now FDA-approved for type 2 diabetes and obesity.
Oral GLP-1s are coming too. Semaglutide is now available as a pill (Rybelsus). It’s not as strong as the injection, but it’s a step toward needle-free treatment.
These aren’t replacements for metformin-they’re upgrades for people who need more.
What’s the future of diabetes treatment?
The days of treating diabetes with just one pill are fading. Today’s approach is personalized. Your doctor doesn’t just look at your A1c. They look at your heart, kidneys, weight, and lifestyle.
Many patients now start with a GLP-1 or SGLT2 inhibitor, then add metformin if needed. Others use them together. Some skip metformin entirely.
The goal isn’t just to control sugar. It’s to prevent complications before they start. That’s why the best treatment today isn’t about what replaces metformin-it’s about what works best for you.
What if I can’t afford the new drugs?
Cost is still a barrier. GLP-1 agonists can cost $800-$1,200 a month without insurance. But many manufacturers offer savings cards. Some pharmacies now sell generic versions of SGLT2 inhibitors for under $20 a month.
Medicare Part D and many private plans now cover these drugs for people with heart or kidney disease. Ask your doctor about patient assistance programs. You might qualify for free or low-cost medication.
Don’t let cost stop you from asking. These drugs can save your life-and your wallet-in the long run.





