Medical Tourism Risks – What You Must Know Before Going Abroad
When considering medical tourism risks, the potential hazards associated with seeking medical care outside your home country, it’s crucial to understand the whole picture. One major threat is counterfeit drugs, fake or substandard medicines that may contain harmful ingredients or wrong dosages. Another is surgical procedures abroad, operations performed in foreign facilities that might lack proper accreditation or experienced staff. All of these are shaped by regulatory oversight, the laws, inspections and standards that govern health services in a destination country. Together they create a web of factors that directly impact patient safety and the overall outcome of any treatment you pursue overseas. Understanding these connections helps you decide where to go, what to ask, and how to protect yourself before you book that appointment.
Why Each Risk Matters
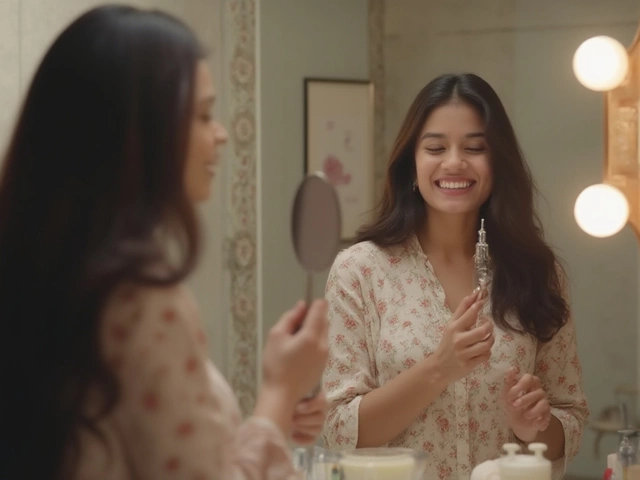
First, counterfeit drugs can turn a weight‑loss plan or chronic‑illness regimen into a dangerous gamble. Imagine ordering a popular injectable like Wegovy from an unverified online pharmacy while you’re abroad; the product might be diluted, contaminated, or completely fake, leading to ineffective results or severe side effects. Second, the allure of cheaper knee replacement surgery may hide gaps in surgeon credentials or post‑op care standards. A rushed operation in a clinic with lax infection controls can cause longer recovery, additional surgeries, or even permanent disability. Third, regulatory oversight varies wildly: some destinations enforce strict quality checks, while others rely on minimal paperwork. Without solid oversight, even reputable hospitals can slip through the cracks, exposing you to subpar equipment or inexperienced staff. Each of these risks doesn’t exist in isolation; they influence each other, making a thorough vetting process essential.
So, how can you turn this knowledge into action? Start by verifying the accreditation of any hospital or clinic you’re eyeing—look for international certifications like JCI or NABH. Cross‑check the pharmacy’s licensing and read reviews that focus on drug authenticity. Ask for detailed post‑procedure care plans and confirm that they align with standards you’d expect at home. Finally, check the legal environment: does the country have a reliable medical board, and what recourse do you have if something goes wrong? By treating each of these steps as a piece of the larger safety puzzle, you’ll lower the odds of falling into a trap of low‑cost but high‑risk care. Below you’ll find articles that break down these topics in depth, giving you real‑world tips and case studies to navigate medical tourism with confidence.

Cons of Medical Tourism: Risks You Should Know
Explore the hidden risks of medical tourism, from safety and legal issues to hidden costs and follow‑up challenges, to help you decide if it’s worth it.