What Is an A1C Test and Why It Matters
If you or someone you know has diabetes, you’ve probably heard the term “A1C” tossed around in doctor’s offices. It’s not a mystery lab code – it’s a simple blood test that tells you how your average blood sugar has been over the past two to three months. In plain words, the A1C number is a snapshot of how well your glucose levels have been controlled without you having to log every single finger‑stick reading.
Why does this matter? Because high blood sugar over time can damage organs, eyes, nerves, and the heart. The A1C test helps catch problems early, lets you and your doctor see trends, and guides treatment tweaks before complications set in.
Reading Your A1C Results
The result comes back as a percentage. A normal range for people without diabetes is usually below 5.7%. If you’re diagnosed with diabetes, the goal is often to keep it under 7%, though your doctor might set a different target based on age, health conditions, and personal risk factors.
Here’s a quick cheat‑sheet:
- 5.7% – 6.4%: Prediabetes – higher risk, but lifestyle changes can pull you back.
- 6.5% or higher: Diabetes – indicates chronic high glucose.
- Below 7% (for diabetics): Good control – lowers risk of complications.
Ways to Lower Your A1C Naturally
Lowering the A1C isn’t about drastic dieting for a week. It’s about steady habits that keep blood sugar stable. Start with your plate: choose whole grains, fiber‑rich veggies, and lean proteins. These foods slow sugar absorption, which keeps spikes in check.
Next, move a little every day. Even a brisk 30‑minute walk after meals can drop glucose spikes dramatically. If you’re new to exercise, start with short walks and build up – consistency beats intensity for A1C.
Don’t forget sleep. Skimping on rest messes with hormones that regulate sugar, pushing your A1C up. Aim for 7‑8 hours of quality sleep, and try to keep bedtime routines calm.
Finally, check your meds. Some drugs raise blood sugar as a side effect. Talk to your doctor before stopping anything, but let them know if you notice your A1C creeping up after a new prescription.
Tracking progress is easy: ask your doctor for the A1C test every three months if you have diabetes, or once a year if you’re monitoring prediabetes. Seeing a lower number after a few weeks of better habits feels rewarding and keeps you motivated.
Bottom line: the A1C test is a practical tool, not a judgment. Use it to guide tiny, everyday changes that add up to big health wins. Keep your meals balanced, stay active, prioritize sleep, and stay in touch with your healthcare team. Over time, those modest steps will bring your A1C down and protect you from the long‑term effects of high blood sugar.

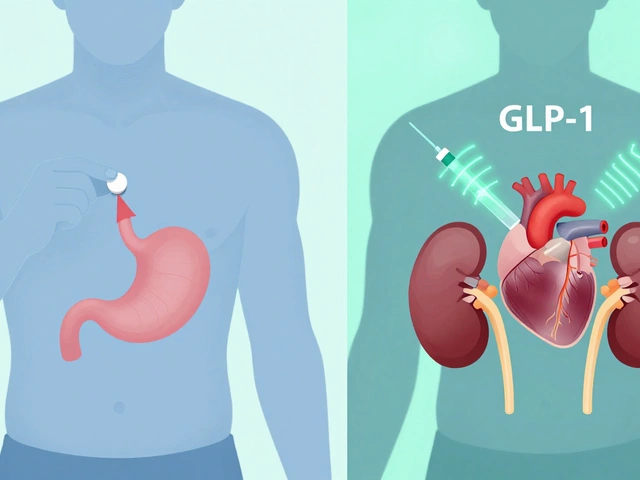
A1C Levels for Ozempic: What You Need to Know
Wondering what your A1C needs to be to get prescribed Ozempic? This article explains the exact A1C threshold doctors look for, what Ozempic is for, and the steps involved if you want to get a prescription—especially through an online pharmacy. Get real-life tips on how to talk to your doctor and what medical records you’ll need. Find out what matters most if you’re thinking about Ozempic for diabetes or weight loss.
Start Metformin at the Right A1C: What You Should Know
Knowing when to start metformin is key for effectively managing type 2 diabetes. This article explores the specific A1C levels that typically indicate the need for this medication. By understanding these indicators and considering your lifestyle, you can make informed decisions about your treatment plan. Insightful tips and reliable information help you navigate your path with ease. It's about taking control of your health with confidence.