If you’ve ever wondered which cancer is the most painful, you’re not alone. People ask this all the time, because pain is one of the scariest parts of a cancer diagnosis. It's not just about the disease itself—it's about how much it can hurt, mess with sleep, and drain energy. Some cancers turn up the pain dial way higher than others, and knowing which ones do it can help you prepare and get the right treatment sooner.
Cancer pain comes in all shapes and sizes. It can feel like a dull ache, a sharp stab, or something you can’t even describe properly. Pain usually ramps up when a tumor presses on nerves, bones, or organs. Bone cancers and some advanced cancers—like pancreatic or head and neck cancer—are infamous for causing severe pain. But it's not just the physical pain; it can wear you down emotionally and mentally too.
The good news? Doctors have come a long way in treating cancer pain. Modern pain relief isn’t one-size-fits-all—you’ve got options, from strong meds to newer, targeted treatments and even simple changes at home. If you or someone you care about is dealing with cancer, it’s worth digging into these options early on. The sooner pain is managed, the better life can feel, even during treatment. Pain is never something you just have to 'put up with.'
- Why Cancer Hurts Differently
- Most Painful Cancers and Why
- Managing Cancer Pain—What Actually Works
- Tips to Talk With Your Doctor About Pain
- Living with Cancer Pain: Real Life Experiences
Why Cancer Hurts Differently
Not every cancer pain feels the same, and that’s because pain depends as much on where the cancer is as it does on what kind it is. Some cancers barely hurt at all at first, while others can get brutal pretty quick. For example, cancers that grow near nerves, like head and neck cancers, or those that spread to the bones, often crank up the pain much more than cancers sitting in soft tissue.
What’s actually causing the pain? Here’s the straight-up science: tumors can press right on nerves, or they can invade bones and organs. Sometimes, it’s the cancer treatment—like surgery or radiation—that messes with nerves or causes swelling, and you feel pain because of that. Even chemo drugs themselves can trigger nerve pain (they call this neuropathy), which feels like tingling, burning, or straight-up stabbing in hands and feet.
Here’s a quick breakdown of what makes most painful cancers sting so much:
- Nerve Invasion: Tumors pressing on or growing around nerves send constant pain signals to your brain.
- Bone Involvement: Cancers that spread to bones or start in bones, like multiple myeloma or bone metastases, are notorious for deep, aching pain. Bones have tons of nerve endings, so any pressure hurts.
- Organ Pressure: A tumor squishing an organ (like the pancreas or liver) can trigger strong pain, especially if it blocks ducts or messes with blood flow.
Ever wonder how common severe cancer pain really is? Check this out:
| Cancer Type | % of People with Moderate to Severe Pain |
|---|---|
| Bone | Up to 80% |
| Pancreatic | 70% - 80% |
| Head and Neck | 60% - 70% |
| Breast (advanced) | 50% - 60% |
So when you hear about someone dealing with cancer pain, remember: it’s not just about the tumor. Where it grows and how it affects nerves and bones can change everything about the kind of pain they feel—and how hard it is to manage.
Most Painful Cancers and Why
Some cancers just hurt a lot more than others. If someone in your family ever struggled with cancer pain, you know it can be intense and non-stop. But why do certain cancers top the list for pain?
Here’s the deal: pain mostly comes from how a tumor grows and what it pushes against. When cancer invades nerves or bones, every little movement can feel awful. Let’s break down a few that regularly show up as the worst offenders:
- Pancreatic cancer: This one is especially notorious. Tumors here sit deep in the belly and often press right up against major nerves. About 8 out of 10 people with advanced pancreatic cancer report moderate to severe pain.
- Bone cancer: Whether cancer starts in the bone or spreads there from another spot, it often makes the bone weak and painful. The pain is usually constant and gets worse at night or during movement.
- Head and neck cancers: Cancers in the mouth, tongue, throat, or jaw hit lots of nerve endings. Everyday things like swallowing, talking, or even breathing can become excruciating.
- Anal and rectal cancers: The pain with these comes from nerve-rich areas and, as the tumor grows, it can cause constant discomfort and sharp pains—especially during bowel movements.
- Lung cancer: If the tumor presses on nerves in the chest wall or spine, pain can travel into the back, shoulder, or ribs. It sometimes feels sharp or deep—kind of like a toothache, but in the chest.
Check out this data showing which cancers are most likely to cause severe pain:
| Cancer Type | % Reporting Severe or Uncontrolled Pain |
|---|---|
| Pancreatic | 80% |
| Bone (Primary or Metastatic) | 70% |
| Head & Neck | 60% |
| Rectal/Anal | 50% |
| Lung | 40% |
No matter which cancer you’re dealing with, pain isn’t just physical. It messes with mood, energy levels, and relationships. But there’s always a reason for the pain, and that means there’s usually a way to treat it or at least dial it down. If you recognize these cancers or their pain patterns, talk to your doctor right away—there are treatments that can make a real difference.

Managing Cancer Pain—What Actually Works
If you’re dealing with cancer pain, you want answers that actually help. The old idea that you just have to "tough it out" is outdated. Today, doctors attack cancer pain from several angles and don’t wait till it’s unbearable. This is a good thing—because the right plan can really take the edge off.
Pain relief for cancer treatment usually works best when tailored to your situation. Here are some of the main options:
- Pain medication—This is where most people start. Simple options like paracetamol or ibuprofen work for mild pain. When pain gets worse, doctors might go up to stronger meds, like opioids (morphine, oxycodone), if needed.
- Nerve blocks and patches—For pain from nerves, doctors sometimes inject meds near the nerve or use patches like lidocaine. These can be great when regular pills aren’t cutting it.
- Radiation therapy—Not just for shrinking tumors, radiation can actually stop pain by shrinking whatever is pressing on nerves or bones.
- Physical therapy—A good physio can teach you gentle moves and stretches. This can help with stiffness and day-to-day pain, especially if cancer or its treatment has messed with your mobility.
- Palliative care—This team is all about making you comfortable. They know every pain-fighting trick in the book and don't just focus on the physical stuff but your mood and sleep, too.
Here’s a quick look at how common pain relief options stack up:
| Treatment | How Fast It Works | Good For |
|---|---|---|
| Painkillers (opioids/non-opioids) | Within minutes to hours | Moderate to severe pain |
| Nerve blocks/patches | Within hours | Nerve pain that won’t settle |
| Radiation therapy | Within days to weeks | Pain from growing tumors, bone pain |
| Physical therapy | Over weeks | Pain from movement, stiffness |
| Palliative care support | Ongoing | Total support, pain plus mood |
Sometimes pain relief is a mix-and-match deal. Maybe you use a patch, take some pills, and add in physical therapy. If pain keeps breaking through, tell your doctor. They can tweak your plan or bring in a pain specialist. You don’t get bonus points for suffering, so be honest about how much it hurts—there’s almost always an answer that works better for most painful cancer symptoms.
Tips to Talk With Your Doctor About Pain
A lot of people feel awkward telling their doctor just how much they’re hurting. Maybe you feel like you should “tough it out,” or you worry the doctor’s too busy to hear details. But getting real about your cancer pain makes a massive difference. Doctors aren’t mind readers, and pain is personal, so sharing the full picture helps everyone make better choices for your care.
Here’s what helps during your next appointment:
- Be Specific: Don’t just say it hurts—try to describe where, when, and how it hurts. For example, “It’s a stabbing pain in my lower back, mostly at night.”
- Use a Pain Scale: Doctors usually use a zero-to-10 scale, where zero is no pain, and 10 is the worst you can imagine. Rating your pain helps them track how things change over time.
- Track Patterns: Does it get worse after treatment? Does anything help, like heat pads or certain meds? Noting patterns gives your doctor clues for solutions.
- Mention Side Effects: If painkillers make you feel sick, dizzy, or spaced out, be honest. There are often other options or ways to manage side effects.
- Bring Notes: Jot stuff down before your visit. When you’re in the moment, details slip your mind. A quick list or pain diary works wonders.
If you’re worried you ask too many questions—don’t be. No question or detail is too small when it comes to cancer pain and pain management. Some folks even bring a friend or family member to help ask what they forget or back them up if the pain gets overwhelming.
| What to Tell | Why It Matters |
|---|---|
| Type & Location | Helps pinpoint source |
| When It Flares | Shows patterns & triggers |
| What Eases/Worsens It | Guides treatment adjustmen |
| Side Effects of Meds | Doctor can switch what’s not working |
One more thing: If your pain changes suddenly or gets worse, let your doctor’s office know right away. Fast changes sometimes call for faster tweaks in your cancer treatment or pain plan.

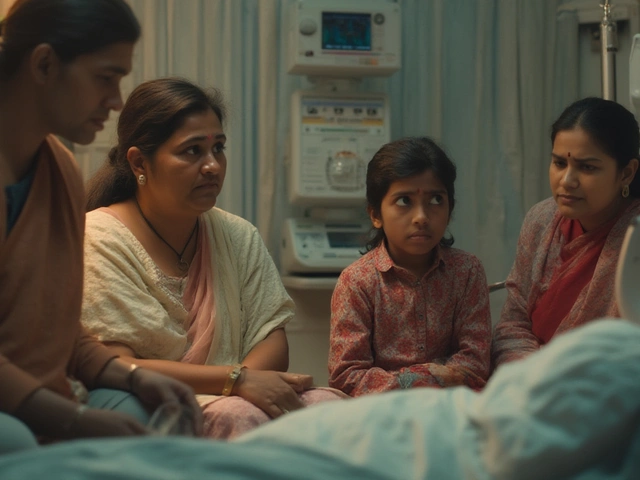
Living with Cancer Pain: Real Life Experiences
Cancer pain is more than just a symptom—it’s a daily battle for way too many people. When my aunt went through pancreatic cancer, she said it wasn’t the diagnosis that kept her up at night, it was the constant ache in her belly and back. That pain colored every decision, from what to eat to whether she even wanted to get out of bed. She wasn’t alone. Studies show about 70% of people with advanced cancer feel moderate to severe pain at some stage. That’s not just a number—you feel it every time you talk to someone fighting cancer pain.
Bone cancers and metastatic cancers can be especially brutal. When cancer spreads to the bones, the pain can flare even with a small movement. One man I met during chemo said, “It’s like toothache in your bones—it just won’t quit.” That’s a pretty common way people describe most painful cancers like bone or pancreatic cancer. Even simple stuff like walking to the bathroom can feel like a marathon.
So, what helps? People who have lived through bad cancer pain say a combination of things works best. It’s rarely just about taking one pill and moving on. Here are a few smart strategies folks have shared, and that pain doctors recommend:
- Pain medications: Start low and go slow, but don’t wait too long. Strong pain needs strong meds. Opioids do have side effects, so it’s important to work closely with your doctor to find the sweet spot.
- Timing is everything: Don’t play catch-up with pain. Take meds regularly, even if you feel okay at the moment.
- Stay honest: You have to tell your doctor exactly what’s going on. Hiding or underplaying pain just slows down real help.
- Try physical therapy or light movement: Weirdly, a bit of gentle movement helps for some. Simple stretching or walking can ease stiffness and lift mood.
- Mental health matters: Pain piles up if you feel helpless or down. Counseling, meditation, or just talking things out helps more than most expect.
The bottom line? Everybody’s pain is unique, especially with cancer treatment. One person with lung cancer might only feel mild discomfort, while another with the same diagnosis is stuck with constant throbbing. What really makes a difference is having a team—doctors, nurses, and family—who take pain management seriously. If medication isn’t cutting it, there are options: nerve blocks, special patches, and even some newer nerve-targeting treatments. Ask, push, and don’t settle for suffering in silence.
| Type of Cancer | Chance of Needing Strong Pain Relief |
|---|---|
| Pancreatic Cancer | ~75% |
| Bone Metastases | ~80% |
| Head and Neck Cancer | ~60% |
| Breast Cancer (Advanced) | ~55% |
I’ve seen families, like mine, find little ways to help too. My wife Neha figured out routines and meal plans my aunt actually liked, and that helped keep her spirits up as the pain got harder to manage. Small wins matter. So, if you’re helping someone with painful cancer, don’t brush off the pain—make it a priority, and keep asking, “What actually makes today easier?” Sometimes, that’s the best therapy there is.