If you’ve ever taken metformin or know someone who does, the first thing that probably comes to mind is: “Is this stuff safe for my organs?” It’s an honest question, and there are a lot of rumors out there—especially about kidneys and the liver. Let’s cut through the noise and get real answers that matter for your health.
Metformin is a go-to drug for type 2 diabetes. Doctors love it because it works well and has a pretty solid track record. But, like every medication, it isn’t perfect. Your organs play a big role in how drugs are broken down and cleared from your system, and metformin is no exception.
One fact to know off the bat—metformin doesn’t mess with your liver the way some people fear. It’s your kidneys that do most of the heavy lifting. If your kidneys aren’t working right, metformin can stick around too long and start causing problems, like a rare but serious condition called lactic acidosis. That’s why kidney health checks are a must before starting—and while taking—metformin.
So, if kidney issues run in your family or you’ve had shaky results on kidney blood tests, don’t ignore it. Talk it out with your doctor. Metformin might still be safe for you, but staying on top of kidney numbers can keep things in check. Stick around as we break down what’s happening in your body, how to spot trouble, and what you can do to stay safe while taking this medicine.
- How Metformin Works in Your Body
- The Main Organ at Risk: What the Science Says
- Signs to Watch Out For
- Ways to Protect Your Health on Metformin
How Metformin Works in Your Body
Metformin, probably the most popular diabetes medication worldwide, isn’t just about “lowering blood sugar” in some mysterious way. Here’s how it actually does the job inside your body.
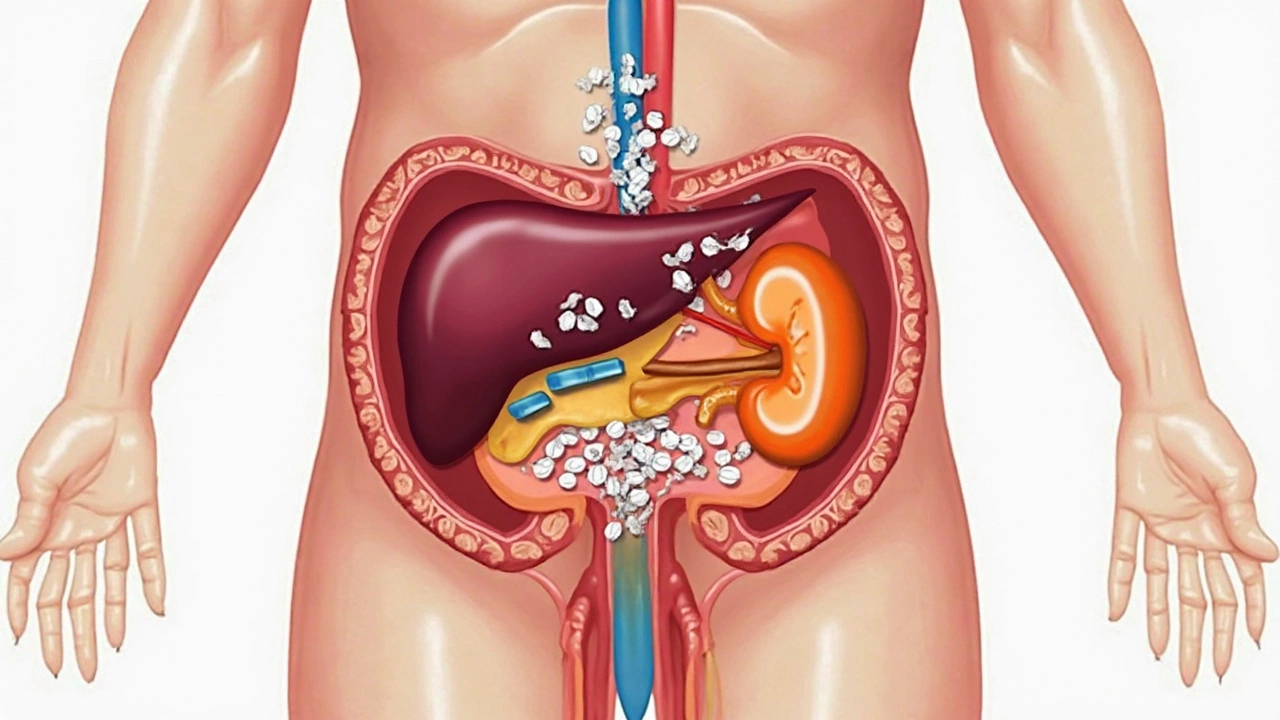
First, metformin mainly helps your body use insulin better. If you have type 2 diabetes, your body either doesn’t use insulin well or doesn’t make enough of it. Metformin tackles this by making your cells respond more efficiently to insulin. It also lowers the amount of sugar your liver pumps out into your blood—most people don’t realize that your liver is always making sugar, even when you’re not eating.
The magic really happens in the liver and muscles. Here’s a breakdown:
- Reduces sugar production in the liver: Metformin tells your liver not to flood your system with glucose (sugar), especially during the night and between meals.
- Makes muscles take up more sugar: It helps your muscles suck in more glucose from your bloodstream, which means less sugar floating around causing problems.
- Improves insulin sensitivity: Your body needs less insulin to get the same job done. This not only helps control blood sugar but can also reduce stress on your pancreas over time.
- Minimal risk of low blood sugar: Unlike some other diabetes medication, metformin almost never causes hypoglycemia (super low blood sugar) when taken on its own.
After you swallow a metformin pill, it passes through your stomach and gets absorbed mostly in your intestines. Then, it travels to your liver and muscles where it goes to work. But get this—metformin doesn’t get broken down by your liver like lots of other meds. Instead, your kidneys filter it out of your blood and flush it away in your pee. That’s why kidney function is a big deal for anyone taking this medication.
To give you an idea of how common metformin is, over 120 million prescriptions for metformin are written each year worldwide. That’s not just a random number—doctors trust it because it does what it says with minimal side effects for most people, as long as the kidneys are up for the job.
So, metformin works mainly by helping your liver and muscles manage sugars better and leans heavily on your kidneys to clear it from your body. If those main players are healthy, metformin usually does a good job keeping your blood sugar under control with few surprises.
The Main Organ at Risk: What the Science Says
The big headline: the organ you really need to watch when taking metformin is your kidneys. Some people think it’s hard on the liver, but research shows the kidneys actually do the heavy work of clearing metformin from your bloodstream. If your kidneys are working like they should, metformin just passes through your system. But when they slow down, that’s when trouble can start.
The main concern is a rare but serious side effect called lactic acidosis. This happens when too much metformin builds up in your blood because your kidneys can’t flush it out as fast as they should. Lactic acidosis is no joke—it can make you really sick in a hurry, with muscle pain, trouble breathing, and confusion. That’s why anyone with kidney problems gets extra attention when doctors prescribe diabetes medication.
Here’s a quick look at how doctors check your risk:
- They’ll order blood tests that show your kidney function, like eGFR (estimated glomerular filtration rate).
- If your eGFR is under 30, doctors almost always stop metformin.
- If your eGFR is between 30 and 45, some doctors may lower the dose or switch meds depending on your other health issues.
Check out this table that shows how metformin dosing changes by kidney function:
| eGFR (Kidney Function) | Can You Take Metformin? |
|---|---|
| Over 45 | Full dose is usually fine |
| 30-45 | Smaller dose, monitor closely |
| Under 30 | Not recommended |
One thing most folks don’t realize is, for people with healthy kidneys, metformin rarely causes major problems. But if your kidneys aren’t working right, it builds up in your body and that’s when risks pop up. Staying on top of those simple blood tests is the biggest thing you can do to dodge trouble.
What about the liver? For most people with normal liver function, metformin doesn’t cause lasting liver damage. But if you already have serious liver disease, your doctor might play it safe and use something else. So, the real focus stays on the kidneys for most people on metformin.
Signs to Watch Out For
If you're taking metformin, paying attention to how your body feels is smart, especially when it comes to your kidneys. Most people handle this diabetes medication well, but there are some red flags that you don’t want to ignore.
The biggest worry with metformin is a rare but serious side effect called lactic acidosis. It's much more likely if your kidneys aren’t working the way they should. But lactic acidosis doesn’t just show up out of nowhere–your body usually gives you some warning signs. Here’s what to keep an eye out for:
- Trouble breathing or feeling short of breath
- Muscle cramps or feeling way more tired than usual
- Upset stomach, belly pain, or vomiting that won’t go away
- Sudden weakness or dizziness
- Feeling cold, especially in your hands or feet
- Slow or irregular heartbeat
If you notice any of these, don’t sit on it—get checked out right away. Lactic acidosis can sneak up fast and needs quick medical help.
Kidney trouble can also show up as swelling in your legs or feet, changes in how often you pee, or pee that looks foamy. If you’re already dealing with high blood pressure or heart issues, staying alert matters even more.
| Symptom | Possible Cause |
|---|---|
| Swelling in legs/feet | Kidney stress |
| Nausea/vomiting | Lactic acidosis or kidney changes |
| Trouble breathing | Lactic acidosis |
| Less urination | Kidney issues |
Even if you feel fine, try not to skip your regular blood tests. They help your doctor track your kidney numbers and catch any issues early, way before you’d notice yourself.
If you ever get seriously dehydrated—like with a stomach virus or bad diarrhea—let your doctor know. Not having enough fluids can push your kidneys into the danger zone while you're on metformin.
Ways to Protect Your Health on Metformin
You might feel a bit uneasy if you’re taking metformin and you’ve heard stories about kidney trouble or other side effects. The good news is, with some solid routines and honest talks with your doctor, most people can use this diabetes medication safely for years. Here’s how you can stack the odds in your favor.
- Keep up with kidney checks: Your kidneys are the main organ that clears metformin from your body. Doctors usually run blood tests for creatinine and eGFR before starting you on it, then check every year (or sooner if you have risk factors). Don’t skip those lab visits—they matter.
- Stay hydrated: Dehydration can make things worse for your kidneys. Drink water regularly, especially if you get sick with vomiting, diarrhea, or a high fever.
- Don’t ignore symptoms: If you suddenly feel super tired, short of breath, confused, or have muscle pains, reach out to a healthcare provider. These could be warning signs of lactic acidosis, which is rare but serious.
- Update your doctors: Always tell healthcare providers (even at the dentist or ER) that you’re on metformin. This is especially important if you need imaging tests with contrast dye—your doctor might tell you to pause your med to protect your kidneys.
Everyday choices can make a big difference if you’re using metformin. Want some numbers? An NHS study in 2023 found that people who had annual kidney tests had a 33% lower chance of metformin-related side effects. That’s a game changer.
| Tip | How Often |
|---|---|
| Kidney function test | 1-2 times a year |
| Discuss all meds | Every doctor visit |
| Hydrate well | Daily |
| Report symptoms | Right away |
Being smart with metformin isn’t about being paranoid—it’s about spotting things early and keeping your kidneys and the rest of you in top shape. No need to ditch the med if it works for you, just play it safe and stay in the loop with your care team.