Knee Replacement Eligibility: Who’s a Good Candidate?
When assessing knee replacement eligibility, the collection of medical and lifestyle factors that decide if total knee arthroplasty is appropriate, doctors balance the severity of joint damage with overall health. The goal is to make sure the surgery will improve function without causing undue risk. knee replacement eligibility is not a one‑size‑fits‑all rule; it’s a checklist that varies by person.
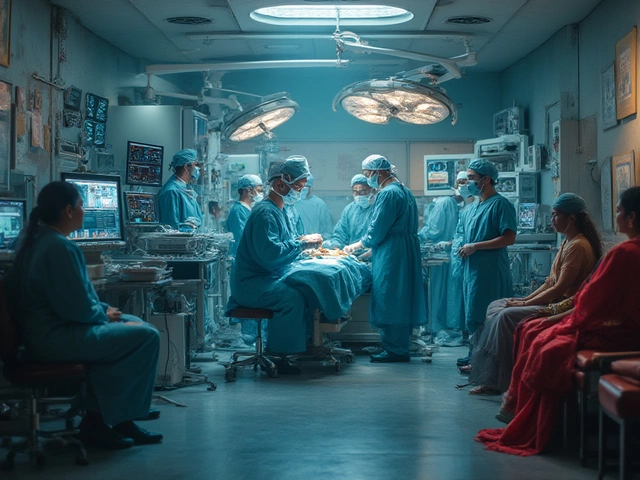
First up is the orthopedic evaluation, a detailed exam that includes imaging, range‑of‑motion testing, and pain assessment. This step pinpoints the exact wear on cartilage and ligaments. Without a solid evaluation, surgeons can’t justify the invasive procedure. The evaluation also reveals whether conservative treatments like physio or injections have been exhausted, which is a prerequisite for moving forward.
Key Factors Influencing Eligibility
Age is a common myth driver, but joint health, the condition of cartilage, bone, and surrounding tissue matters more. Patients in their 50s with severe osteoarthritis may qualify, while a healthier 70‑year‑old might wait if their joint wear is mild. Body mass index (BMI) also plays a role: higher BMI stresses the new implant, raising the risk of early failure. Doctors often advise weight loss before surgery to improve outcomes.
Comorbidities such as diabetes, heart disease, or severe osteoporosis can tip the scales. These conditions increase infection risk or affect bone quality, influencing the decision. In many cases, a multi‑disciplinary team reviews labs, imaging, and lifestyle factors to create a personalized risk profile. This collaborative approach ensures that the surgery’s benefits outweigh potential complications.
Recovery expectations are woven into the eligibility conversation. post‑operative recovery, the period of rehabilitation and physical therapy after knee replacement demands commitment to exercises and follow‑up visits. If a patient cannot commit to the rehab schedule—due to lack of support or mobility issues—the surgeon may suggest alternative treatments. Understanding the rehab timeline upfront helps set realistic goals and prevents disappointment.
Insurance and cost considerations also affect who gets the surgery. Many policies require documented failure of non‑surgical therapies before approving a knee replacement. Providing clear evidence from the orthopedic evaluation and a detailed treatment history speeds up approvals. Patients who navigate these administrative steps early often experience smoother scheduling.
Bottom line: eligibility hinges on a blend of imaging results, functional limitations, overall health, and the willingness to engage in a structured rehab program. Below you’ll find articles that break down each of these elements, from how BMI influences outcomes to what to expect in the first weeks after surgery. Use the insights to have an informed conversation with your doctor and decide if knee replacement is right for you.

Bad Candidates for Knee Replacement: Who Should Avoid Surgery?
Learn which medical and lifestyle factors make someone unsuitable for knee replacement, how to assess eligibility, alternatives, and steps to become a better candidate.

Best Medicine for Diabetes: Discover Your Options
Mar, 28 2025

Can You Safely Take Multiple Vitamins Together?
Jan, 23 2025